Women have a lot of things to juggle in their lives. Children, careers, travel, a healthy diet and exercise all take a good deal of time and effort to manage. However, after a certain age (and even sometimes before) one very important thing needs to be added to that list; being proactive when it comes to breast health.
In light of Breast Cancer Awareness Month, we sat down with Dr. Mark Goldshein to get the facts and need-to-knows!
So first of all, are you wondering what age you should begin getting screened? Per Dr. Goldshein, “The radiologists at Derry Imaging Center conform to the recommendations of the American College of Radiology, the Society of Breast Imaging, and multiple academic cancer centers, which is to have, for an average-risk woman, annual mammography starting at age 40, and continuing for as long as the woman is in good health. Mammography for breast cancer screening is the only test for breast cancer that has been shown in randomized clinical trials to decrease the mortality rate of breast cancer by at least 30%. Since those trials were done decades ago, and the technical nature of mammography has advanced considerably since then, it’s likely that the mortality reduction is even larger in the current era.”
When you do choose to get screened, your first exam will be considered your baseline screening. “Baseline screening is the first mammogram of the patient’s life, and assumes that there are no breast-related symptoms or signs (no masses or lumps, no focal pain, no nipple discharge, no nipple retraction, no skin changes, etc.),” said Dr. Goldshein.
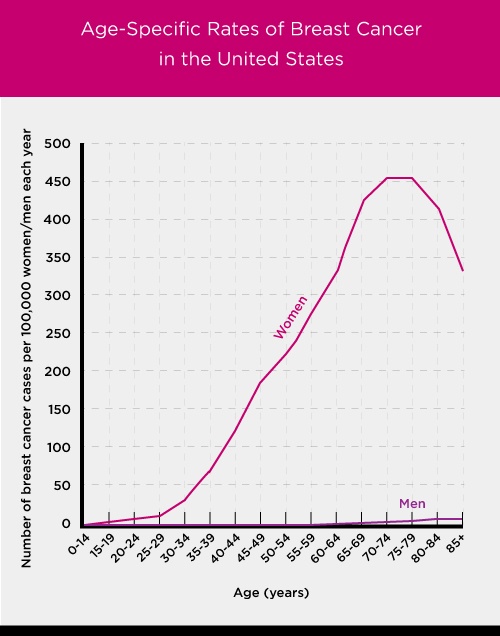
We now assume you are wondering why average risk women should start screening at 40. Well, it’s simple! Risks increase with age.
“There is increasing risk of being diagnosed with breast cancer as a woman ages,” confirmed Dr. Goldshein. Dr. Goldshein was kind enough to provide us with a resource to help women learn more facts. It can be accessed here.
One of the major reasons women don’t get screened is due to perceived false positives. As to that, Dr. Goldshein said, “Screening risks are in the eye of the beholder. Some women are quite concerned with ‘false positive’ results, and the more one is screened, for any disease, the more likely one will have something that requires more evaluation. Our experience, though, is that most women will take the risk that they might get called back for additional imaging in the hope that if they should develop a breast cancer, we would increase the likelihood of finding it as early as possible.”
Of course, false positives are a real risk, but that’s true of any system (even if it’s the best one available). Dr. Goldshein said, “Mammography is imperfect, but it’s the best test available for screening. There is a substantial overlap between the appearance of many cancers and many different benign processes in the breast. It is this overlap which requires further evaluation, either with additional imaging exams (more mammographic views, ultrasound, and/or MRI) or with clinical evaluation and short-interval follow up mammography. Biopsy of those abnormalities that have a greater than 2% chance of being cancer is indicated.”
Mammography is the most valuable resource when it comes to typical screening for breast cancer, but there are others such as MRIs available depending on additional risk factors. “Mammography is the cornerstone of any breast cancer screening program. It’s the one exam that has been shown in randomized controlled trials to reduce the mortality of breast cancer. We recommend that all average-risk women have annual screening mammography beginning at age 40. If a woman is known to be at high risk (a known mutation in a breast cancer-associated gene such as BRCA1 and BRCA2, a strong family history of breast cancer with multiple first-degree relatives with breast cancer, etc.) then yearly MRIs should be considered, alternating every six months with mammography,” said Dr. Goldshein.
It is important to do your research when it comes to breast cancer. Dr. Goldshein said, “The screening controversy has created enormous confusion for the general public as well as for many referring health care providers. There are many resources available online. Here’s one that sums it up well.”
So the real question is…should get screened? “I think that every woman should make her own choice. Autonomy is key in all medical decisions. One could easily argue that even though one of eight women is likely to develop breast cancer at some point in her lifetime, the other way to look at this statistic is that 7 out of 8 won’t. Having said this, I make sure that my wife and my sister get their annual screening mammograms. And another misconception that should be dispelled: most (at least 75 or 80%) of breast cancers develop in women who have no family history of breast cancer,” noted Dr. Goldshein.
So based on these responses and our extensive history as a premier imaging center, we do think that yes, you should choose to screen. The best defense is a great offense and we can help you.



